Prof. Xiulan Zhang's team provides new classification of visual field abnormalities in highly myopic eyes without pathological change
Source: Zhongshan Ophthalmic Center
Edited by: Zheng Longfei, Wang Dongmei
On March 12, 2022, the top journal in the field of Ophthalmology -
Ophthalmology published the original research “Classification of Visual Field Abnormalities in Highly Myopic Eyes Without Pathological Change” provided by Professor Xiulan Zhang's team in Zhongshan Ophthalmic Center, Sun Yat-sen University. The article provides a standard for classification of visual field (VF) for the diagnosis, treatment and follow-up of the current growing high myopia combined with glaucoma. It is the third original article published by Professor Zhang's team in the
Ophthalmology since last August.
The prevalence of high myopia has markedly increased worldwide. Projections estimate that the global prevalence of high myopia will increase from 163 million people in the year 2000 to 938 million in 2050, corresponding to 2.7% and 9.8% of the world population, respectively. Patients with high myopia have an increased risk of visual impairment and legal blindness worldwide. It has been estimated that the odds ratio for eyes with high myopia to develop primary open-angle glaucoma (POAG) is about 6 as compared with eyes without high myopia, and that the prevalence of glaucomatous optic neuropathy can be as high as 30% in highly myopic eyes.
However, the early diagnosis of glaucoma in eyes with high myopia is challenging, and there lacks a standard treatment regimen. Therefore, in 2019, Professor Zhang led and jointly established the Glaucoma Suspects with High Myopia study group (GSHM) with 12 top experts in high myopia, glaucoma and epidemiology in 7 countries. And with the support of the Clinical Research Center of Zhongshan Ophthalmic Center and the High-level Hospital Construction Project, Zhongshan Ophthalmic Center, Sun Yat-sen University, two leading clinical studies were conducted simultaneously. One is a prospective cohort study of high myopia with glaucoma (ClinicalTrials.gov, identifier: NCT04302220, BMJ Open 2020; 10: e039183; 1,500 participants included currently); the other is a randomized controlled trial of high myopia with glaucoma (ClinicalTrials.gov, identifier: NCT04296916; Trials 2020 Sep 29; 211(1)). It intends to provide an evidence-based medicine proof for the early detection, diagnosis and treatment of patients with high myopia and glaucoma in the series of studies. At present, over 10 relevant peer-reviewed articles have been published, and one invention patent has been granted.
As the part of the GSHM series of studies, the current study proposes a new and reproducible classification system of VF abnormalities for non-pathological high myopia, based on observation of the 1893 VF reports, literature review, and multiple consensus meetings. The new classification system consisted of four major types and 10 VF patterns (Figure 1), including normal, glaucoma-like defects (paracentral defect, nasal step, partial arcuate defect, arcuate defect), high myopia-related defects (enlarged blind spot, vertical step, partial peripheral rim, non-specific defect), and combined defects (nasal step with enlarged blind spot). The validation of our proposed classification system for VF defects showed relatively good agreement (kappa value ≥0.86). Based on the new visual field abnormalities classification, we found that the normal VF was the most frequent one (74.1%), the glaucoma-like defects and the high myopia-related defects were the next most common types (10.8% and 15.0%, respectively), and the combined defects was the least common type (0.1%) (Figure 2). This system provides a tool for clinician to distinguish glaucomatous VF loss from non-glaucomatous VF defects in highly myopic eyes in their clinical practice and also may facilitate comparison of findings among clinical trials and epidemiologic studies. Since 25.9% (10.8%+15.0%+0.1%) of non-pathological high myopia eyes with VF defects and without obvious symptoms, our future study will focal on these patients and report the follow-up perimetric examinations, to provide evidences for the early treatment.
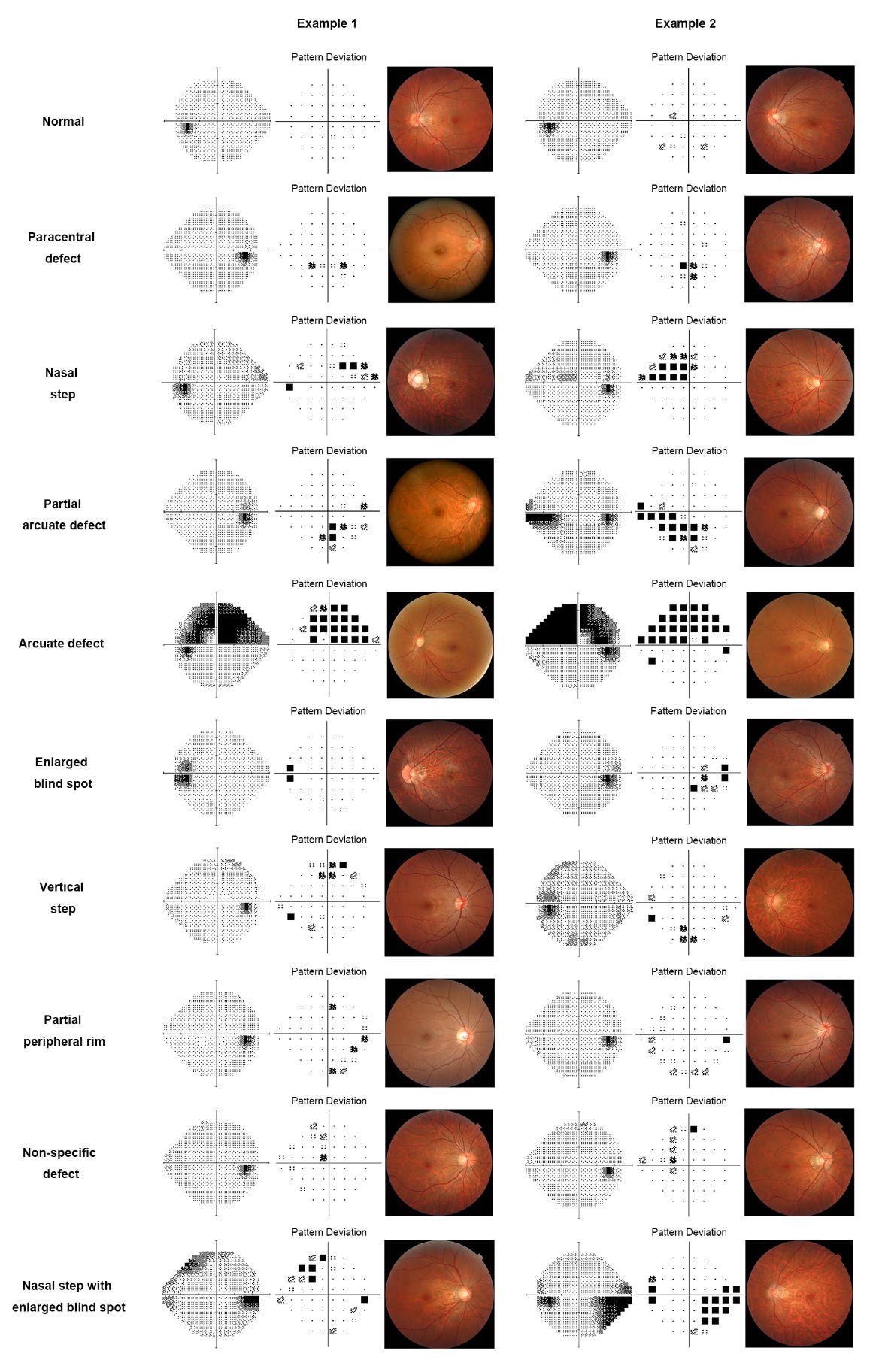
Figure 1. Examples of the new visual field abnormality classification with the corresponding fundus photo.
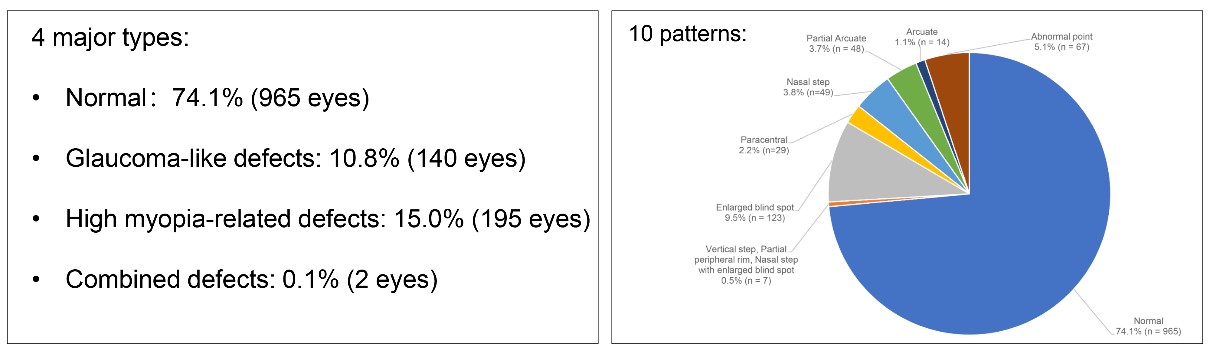
Figure 2. The frequency distribution of the four major types and 10 VF patterns
Dr. Fengbin Lin and Dr. Shida Chen from Zhongshan Ophthalmic Center, Sun Yat-sen University were joint co-first authors; Professor Xiulan Zhang from Zhongshan Ophthalmic Center, Sun Yat-sen University (the final corresponding author), Professor Robert N. Weinreb from Shiley Eye Institute, University of California San Diego, United States, and Professor Jost B. Jonas from Medical Faculty Mannheim, Heidelberg University, Germany and Institute of Molecular and Clinical Ophthalmology Basel, Switzerland were joint co-corresponding authors. State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangdong Provincial Clinical Research Center for Ocular Diseases was the first affiliation.
Link to the article:
https://www.aaojournal.org/article/S0161-6420(22)00193-2/fulltext#relatedArticles
